Medical information is reliable Checked by Eremin Alexey Valentinovich
Lack of memory for certain events is called amnesia. It does not always indicate a pathological process; for example, many cannot reproduce the first years of childhood. But most often, amnestic syndrome indicates the presence of a number of neurological or mental abnormalities. According to statistics, 25% of people on Earth suffer from memory impairment to one degree or another.
Classification
Depending on the degree of memory loss, amnesia can be complete or partial. In the first case, a person cannot remember anything from a period of his life, and in the second, he observes vague fragments of events. There is also selective or local amnesia, when the patient loses only a specific skill. This condition is characteristic of psychogenic disorders. According to the time of forgetting, this deviation can be:
- retrograde in the absence of memory for everything that happened before the onset of the disease;
- anterograde, when everything that happens after the first signs of the disorder is forgotten;
- combined (combines retrograde and anterograde amnesia);
- fixation – forgetting what is currently happening, usually lasts for 2-5 minutes.
The type of course of amnestic syndrome can be:
- regressing with gradual recovery;
- stationary, in the absence of positive dynamics and without signs of deterioration, forgetting usually applies only to a certain situation;
- progressive – gradual loss of memory up to its complete loss.
There is also retarded memory loss, when a person’s events are erased some time after stress, acute psychosis or traumatic injury. Immediately after regaining consciousness, he talks about what happened, but later forgetting sets in.
Cases of vascular dementia
Scientists have established for certain that the Russian writer, imperial maid of honor Smirnova Alexandra Osipovna, whom A.S. once admired. Pushkin, suffered from vascular dementia.
From her youth, she was distinguished by her gloomy mood or its swings, insomnia. At the age of 40, she suddenly lost weight and became haggard. I didn’t want to see doctors. She was treated on her own: sermons, rituals. Her heredity was burdened with mental disorders.
At the age of 69, her condition worsened further. Her speech became incoherent, she rearranged syllables in words and distorted them. Memory suffered and behavior was disrupted. The mental state deteriorated sharply, reaching the level of mental disorder.
According to data collected from eyewitnesses, Alexandra Osipovna was diagnosed with “atherosclerotic dementia.”
Another famous writer, the author of Uncle Tom's Cabin, Harriet Beecher Stowe, was also diagnosed with vascular dementia. She devoted her entire life to caring for her large family, fighting poverty and disease. In the last years of her life, after the death of her husband, Harriet lived completely alone. She exhibited strange behavior. Sometimes she came to Twain’s house and wandered around the rooms there. She didn’t pay attention to anyone, she was aloof. After walking around a bit among the people, she returned home. Her mental abilities had completely deteriorated, she practically could not take care of herself. The patient's memory underwent special destructive changes.
Transient and permanent amnesic syndrome
Transient amnesia is observed with a number of deviations associated with various factors, it happens:
- Transitional global. It is observed in middle-aged and elderly people, more often in males, and lasts for several hours (from 4 to 12). In this case, patients do not lose their identity, but they experience confusion. However, there is no evidence of cerebral ischemia. During the study, the patient demonstrates a profound loss of memory for all events occurring at the time of the attack. A return to the original state is observed within 1-2 weeks to 2-3 months.
- Transitional epileptic. Occurs in patients with epilepsy, sometimes amnestic syndrome manifests itself as the first sign of the disease before the onset of seizures.
- Injuries and head injuries. Typically, after a TBI, an episode of temporary retrograde amnesia is observed; the longer it lasts, the more negative the prognosis, and the likelihood of cognitive impairment, mental disorders, and social problems increases. Post-traumatic syndrome also includes anxiety, irritability and complaints of somatic pathology.
- Alcohol blackouts. Memory lapses associated with alcohol abuse mean that a sober person cannot remember events when he was drunk. But after drinking a strong drink, they easily return.
Complete memory loss is observed in progressive diseases that cannot be completely cured. This happens with dementia, mental illness, inoperable brain tumor and other disorders. Therapy in this case is to stop the deterioration of the condition and take measures to adapt the patient to his amnesia.
What causes disorientation?
Consciousness loses the correct mood, disorientation occurs due to disturbances in the functioning of the central nervous system. The causes are considered to be the consequences of mechanical head injuries or infringement of the brain by a cancerous tumor, blood accumulation or vasodilation. A state of disorientation and confusion is one of the symptoms of many ailments.
Possible causes of disorientation:
● Mental illness; ● Epilepsy; ● Alzheimer's syndrome; ● Metabolic disorders; ● Insufficient amount of oxygen in the blood; ● Kidney problems; ● Inflammation of the brain; ● Hypoglycemia.
In older people, mental disorientation is most often one of the signs of advancing insanity. A similar condition, disorientation syndrome, can occur in children of primary school age against the background of stressful situations. Loss of orientation occurs with dehydration, overheating or hypothermia, as well as with the use of psychotropic drugs, alcohol, and after anesthesia.
Manifestations of amnestic syndrome
A classic sign of amnesia is the inability of a person to recall a certain period of time in his life. Most often, recent events are forgotten first, and then more distant ones. In a regressing process, recovery is observed in the reverse order. Some types of disorder involve false, fictitious memories, or confabulations. With their help, the body tries to fill the gaps. At the same time, the person sincerely believes in the truth of his “memories.”
Amnestic syndrome after a stroke is characterized by hypo- and paramnesia (general memory loss and confusion of present and past events). At the same time, speech impairment and movement deficits are noted. Memory loss occurs in psychoorganic syndrome, and cognitive dysfunction is also observed. A person loses the ability to assimilate new information, his attention decreases, and his thought processes slow down. With dissociative amnesia, the patient becomes absent-minded, begins to wander, and often experiences affective disorders. Transient global loss of memories is characterized by complete disorientation. With Korsakoff's syndrome, several types of amnesia are often combined.
With a stationary disorder, a person often suffers and worries about his condition, is tormented by a feeling of guilt, and becomes depressed. Progressive amnestic syndrome leads to complete helplessness; a person can leave home and get lost in a familiar area. There is a gradual loss of skills and knowledge. At the end there is complete disorientation and constant care is required.
Neurological disorders
In the initial stage of the disease, neurological dysfunctions manifest themselves as general symptoms. Weakness and fatigue, absent-mindedness, and irritability appear. I am bothered by systematic headaches and sleep is disturbed. There is an unstable emotional background. Depressive states are possible. The person is unrestrained, hot-tempered, and embittered. Emotional incontinence usually manifests itself in violent crying or laughter, weakness.
Among other neurological indicators, cerebellar syndrome occurs, characterized by uncoordinated movements. It seems that the arms and legs are moving chaotically. Because of this, the gait changes: it becomes shaky, slack. The person appears to be drunk. Instability of the step provokes falls.
The disease causes accentuation of personality traits. For example, if previously a person was scrupulous and meticulous, then pathology turns him into a picky grumbler.
Pseudobulbar syndrome is expressed by a triad of signs:
- dysarthria - pronunciation disorder;
- dysphonia – loss of voice sonority;
- dysphagia – problems with swallowing.
There are cases of paralysis and paresis, but quite rarely. Muscle tone and reflexes are increased.
Quite often, malfunctions in the functioning of the pelvic organs occur, and epileptic seizures occur.
In general, dementia of vascular origin is characterized by narrowness and fixation of mental processes, loss of flexibility of thinking, fading of cognitive abilities, and a narrow range of interests.
Organic amnestic syndrome
The causes of organic amnestic syndrome can be various lesions of brain tissue: cerebral arteries, white matter, nerves or cerebral cortex. It also leads to the appearance of hematomas and hemorrhages in the central nervous system. The cause of the deviation is sometimes carbon monoxide poisoning with massive brain damage.
When the functions of the temporal regions are disturbed, as happens with epilepsy, they also lead to the fact that a person develops amnestic syndrome. Its causes are:
- malignant tumors, especially when the ventricular walls are damaged;
- Alzheimer's disease and other types of dementia (Lewy, Creutzfelt-Jakob, atherosclerosis and other pathologies);
- Wernicke's disease;
- herpetic encephalitis;
- tuberculous meningitis in severe form;
- transient ischemic attacks (lead to temporary amnesia).
Another common cause of amnestic syndrome is alcohol addiction. Many have noticed that short-term memory loss occurs when intoxicated. Experts associate it with a lack of B vitamins, since ethanol is their antagonist.
Treatment of alcoholic amnesia in our clinic always includes a full course of therapy for this disease with the addition of drugs to improve cognitive and mnestic functions.
Causes of senile dementia
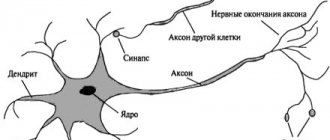
In every person, neuronal activity deteriorates with age. This is due to the natural biological processes of aging. Hormonal levels change significantly, the sensitivity of neural connections decreases, and the brain loses the ability to normally absorb the entire spectrum of nutrients it needs. Senile dementia is a similar process, but occurs in a more active and rapid form.
The main provoking factors of the disease:
- Other diseases of the brain and nervous system (infectious and non-infectious). Act as a catalyst in which neurons lose the ability to fully absorb micronutrients.
- Vitamin deficiency. In particular, B-group, folic acid.
- Kidney, liver, heart failure. Accompanied by disruption of the normal functioning of the vascular system, a smaller volume of oxygen and nutrients is transported to the brain, which causes destructive processes in the cortex.
- Hormonal imbalance.
- Genetic factor. Often this disease is diagnosed to those who already have (had) relatives with the same diagnosis
In about 60% of cases, people with dementia also have Alzheimer's disease.
Cognitive amnesic syndrome
The word “amnesia” itself, translated from Greek, means memory loss, which greatly affects a person’s cognitive abilities. Memorizing events and information is the basis of learning and the emotional coloring of what happened. That is why amnestic syndrome is very traumatic; it not only reduces the patient’s quality of life, but also affects his loved ones.
This condition is considered as a complex of symptoms under various diagnoses. But clinical medicine allows it to be indicated as an independent disease if the cause of the disorder cannot be identified. Typically, amnestic syndrome has two characteristic features:
- loss of memory for past events (retrograde amnesia);
- inability to remember current information (anterograde amnesia).
Other functions of cognition in this case are rarely affected, but may be impaired because they depend on the patient’s memory:
- ability to concentrate;
- organization in space;
- abstraction (visual or auditory).
A person ceases to show initiative and independence, and is almost always in a complacent state. Immediate memory with repetition of just spoken phrases or series of numbers is retained. Some patients in the acute phase of the disease develop a tendency to invent answers or events. With dementia, the patient sometimes replaces lost information about himself with information that he once saw or read. At the same time, adventures are presented to them as their own, but this is done unconsciously.
What is a confused state?
In this process, the ability to think at an average speed disappears, the clarity and consistency of thoughts is significantly destroyed.
Content:
- What is a confused state?
- Causes
- Symptoms
- What is disorientation?
- Current of development
- Medical classification
- Symptoms of the disease
- Benefits of diagnostics
Signs of the disorder are problems with orientation in space and deterioration of attention. Logical thinking disappears and memory is degraded. The highest signs of the psyche change one by one. For example, only speech recognition may be affected. Memory problems are noted, spatial orientation is impaired. There are two types of confused consciousness, depending on the cause of its occurrence - fast and slow.
Manifestations can be one-time or permanent. Dementia and delirium are signs of the latter condition. The integrative function of thinking at the moment of confusion is absent. Along with the expected change, the patient is often silent, moves little, and is depressed outwardly. Illusions and hallucinations accompany the disease. The first arise because the body incorrectly perceives the stimulus, while hallucinations manifest themselves independently. Each person suffers from the disease differently - the determining factor is the underlying cause of the development of the disorder. Slowness of thinking and inconsistency of logical series are emphasized during the first minutes of conversation. Even non-professionals can notice the initial symptoms.
Psychotherapists divide delirium into several classifications: hallucinatory (the ability to see non-existent information); manic (obsession with aggression); catatonic (inability to fully move); confabulatory (twisting of an obvious fact).
Psychogenic amnesia
Conditions that lead to the loss of memory of a certain part of data about one’s personality are called psychogenic. These types of amnesia include:
- Katathimnaya. The patient forgets only those data that are in some way related to psycho-emotional experiences.
- Hysterical. Often observed in hysterical psychopathic syndrome. In this case, the person cannot remember only the traumatic moment.
- Post-hypnotic. The patient is unable to reproduce what happened to him in a trance state. This is usually part of the suggestion.
- Dissociative. Refers to the body's protective reactions that do not allow the destruction of mental functions. Memory for events that cause severe stress is erased. It differs from other types of psychogenic amnesia in that the loss itself is a treatment and relief from further problems.
- Dissociative fugue. Also refers to defense mechanisms, but at the same time a person escapes from a difficult situation by moving to another city and forgetting about his past life and his personality. At the same time, he retains his basic skills completely. After some time, events are restored, usually this happens suddenly and immediately.
Symptoms
The disease in the initial stages is accompanied by the following symptoms:
- Impaired functioning of short-term and long-term memory. The patient may forget recent events that happened to him, the names of relatives.
- Planning daily tasks is difficult for the patient.
- Disorientation in space. The patient may suddenly forget his own neighborhood, even if he has lived in it most of his life. Disorientation in time is less common. A person literally cannot remember what year it is.
- Absent-mindedness. The patient forgets to turn off the lights, leaves things in places that are not at all intended for this.
- Sleep problems.
- Lack of predisposition to learn even simple new skills.
At later stages, the patient experiences:
- regular headaches;
- hallucinations (both visual and auditory);
- problems with speech, writing, reading;
- sloppiness (a person stops taking care of himself).
The above are common signs of dementia. But each patient’s clinical picture is individual.
Diagnostics
Diagnosis of amnestic syndrome requires the participation of several specialists, depending on the basic picture of the disease. A neurologist, narcologist, neurosurgeon, and infectious disease specialist are involved in the work, and if necessary, a psychiatrist is consulted. To determine pathology, the following is used:
- Study of the medical history based on data from a survey of the patient and his close relatives, as well as provided medical documentation.
- Assessment of the state of the nervous system. It helps to determine the presence or exclude organic brain damage and the consequences of traumatic brain injury.
- Mental state assessment. It is performed in people with suspected psychogenic amnesia and symptoms of a mental disorder.
- Studies of the characteristics of the blood circulation of the central nervous system in case of probable vascular disorder. For this purpose, REG, ultrasound examination of the vessels of the head, and MRI are performed.
- In case of traumatic brain injury, a CT or MRI of the brain is prescribed. These methods help to accurately determine the presence, size and location of a tumor, hematoma, tissue degeneration, and lesions after a stroke.
- EEG is used to determine abnormal electrical activity in the brain during epileptic seizures.
- Laboratory tests of blood and urine. Allows you to conduct a drug test, determine the level of vitamin B1, and the presence of toxic substances in the body.
- Study of cerebrospinal fluid. Sampling of cerebrospinal fluid and its analysis is used in cases of infectious origin of amnestic syndrome or intracranial hemorrhage.
Dr. Isaev’s clinic has all the conditions for a full examination of a patient who has lost his memory. The hospital is equipped with modern equipment and a laboratory. If necessary, it is possible to conduct consultations with experienced specialists in any field of medicine.
Forms of vascular dementia
The brain provides us with conscious existence, being responsible for mental, emotional, and adaptive processes. Its substance is strictly structured. Each of its departments is responsible for its functions.
However, any part of the brain can undergo destructive changes, as a result of which a certain type of activity is disrupted. Based on this, several forms of the disease are distinguished, differing not only in location, but also in the caliber of the affected vessels.
Dysmnestic or lacunar dementia occurs against the background of destruction of small-diameter vessels. As a result, multiple infarct foci appear in the thickness of the white and gray matter. This is the most classic variant of the course of the disease, in which all pathological manifestations are not clearly expressed. There is a measured decrease in intellectual abilities, mild memory impairment, and slight slowness of psychomotor skills.
The multi-infarction form is accompanied by damage to vessels of medium diameter, and usually develops in non-acute pathological processes. Its manifestations are insignificant and go unnoticed for a long time even by the patient himself. Its course is gradual. The disorders first progress and then freeze at a certain stage until the next micro-stroke. Among the symptoms of this type of disease, cognitive impairment comes to the fore. Neurological and emotional disorders gradually develop.
Subcortical vascular dementia is a disease of small vessels, against which atrophy of white matter cells occurs with the formation of ischemic areas. Scientists see the reason for this process in the accumulation of amyloid in the walls of the arteries, followed by its inflammation. The clinical picture of the disease is somewhat atypical. It can occur as Alzheimer's disease or as isolated dementia.
Autoimmune vasculitis, such as systemic lupus erythematosus and panarteritis, cause another form of the disease - cerebral vasculitis. It is expressed by dementia and confusion. As a rule, it affects patients over 50.
Mixed dementia combines two forms: vascular and atrophic, that is, Alzheimer's type. Therefore, in the picture of the disease one can observe symptoms of both vascular dementia and Alzheimer's disease, but the latter prevail over the former.
Treatment of amnestic syndrome in Moscow
The goal of helping a patient with memory loss is to restore it or stabilize the condition and achieve long-term remission. Amnestic syndrome does not have a specific treatment regimen. Each patient receives an individual care plan. It depends on the cause of the development of the disorder and the characteristics of its manifestation. For the organic form, medications or surgery are used primarily, and for the psychogenic form, psychotherapy is used. The most commonly used drugs are:
- vascular agents to reduce blood viscosity and expand the microvasculature and improve cerebral blood flow;
- neuroprotectors, nootropics and antioxidants to improve metabolism in brain cells, reduce their sensitivity to ischemia, and normalize cognitive functions;
- anticholinesterase drugs and ginko biloba preparations for dementia in order to reduce the progression of dementia in the elderly and increase daily activity;
- In Alzheimer's disease, memantines are used to improve mnestic functions.
For patients with mental disorders, antidepressants, antipsychotics, tranquilizers, and mood stabilizers are used. They help normalize behavior, restore control over the biological rhythm, improve mood during depression, and eliminate anxiety, phobia, and anxiety.
Dr. Isaev’s clinic uses only proven, certified drugs with minimal side effects. They must be taken strictly according to the course prescribed by the doctor.
If a tumor, hematoma or cyst is detected in the brain, it is surgically removed. Methods of psychotherapy allow, in combination with medication, to accelerate the recovery of the patient’s memory. In the absence of organic disorders, hypnotherapy helps to restore memories. These patients use a cognitive-behavioral technique that allows them to identify negative mental dogmas and replace them with positive ones. With its help, a person relates to his problem more easily and this helps him speed up his recovery.
With the psychogenic form of amnesia, the goal of treatment is not so much to restore memory, but to help the patient accept its loss. The method of psychoanalysis eliminates psychotraumas coming from early childhood, and family therapy improves relationships between loved ones and helps optimize the prognosis for amnestic syndrome. For people with a lack of inclination to demonstrate their feelings and experiences, creative types of treatment in the form of art therapy and fairy tale therapy help. Help for alcoholics with amnesia is provided in the form of the use of vitamins and means for detoxifying the body.
Dizziness - symptoms and treatment
Diagnosis of dizziness is based primarily on the collection of complaints, anamnesis (history) of the disease and clinical examination.
Collection of complaints and anamnesis
Basic questions that can be asked to a patient with acute dizziness:
- How and when did the dizziness start?
- How long does it last?
- What character, in the patient’s opinion, is dizziness (systemic, non-systemic, presyncope).
- Are there certain factors that provoke dizziness (turning the head or body, standing from a horizontal to a vertical position, being in crowded or noisy places, etc.).
- Is dizziness accompanied by pain (headache, chest pain, ear pain), hearing loss, noise in the ears or in the head.
- Are there any accompanying symptoms (double vision, difficulty swallowing, speech disorders, weakness in the limbs, nausea and vomiting) [1].
Physical examination
When examining a patient, the presence and characteristics of nystagmus, the presence of gait disturbances, the performance of coordination tests and stability in the Romberg position (standing with feet together, eyes closed and arms extended in front of you) are first assessed.
Evaluation of nystagmus. In order to correctly distinguish peripheral from central vertigo during the diagnostic process, it is important to determine the nature of the nystagmus. For this purpose, special Frenzel glasses are used: in them, it is difficult for the patient to fix his gaze on any object, which allows him to determine without distortion exactly how nystagmus manifests itself.
Differential diagnosis of peripheral and central dizziness:
- With a peripheral origin, nystagmus is usually horizontal or horizontal with rotational movements of the eyeballs, unidirectional and directed towards a more active labyrinth. When the gaze is fixed, the nystagmus decreases.
- In the case of central origin, nystagmus can be horizontal bidirectional (left-sided when looking to the left and right-sided when looking to the right), vertical or rotational. When fixing your gaze, it may decrease slightly, but, as a rule, does not change.
Positional tests are carried out at the appointment and help determine the cause of systemic vertigo and differentiate positional nystagmus from central nystagmus. The most commonly performed test is the Dix-Halpike test. The patient, who is sitting on the couch, is turned 45° to one side and quickly placed on the couch so that the head is thrown back over the edge of the couch. The doctor monitors the appearance of nystagmus, and the patient reports on his well-being. In the same way, the test is repeated with the head turned in the other direction.
If the answer is positive, it is possible to identify the most common cause of true dizziness, BPPV, and determine in which of the semicircular canals the otoliths causing dizziness are located [18]. With the appearance of nystagmus and dizziness, the most common localization of otoliths is revealed - the posterior semicircular canal.
Assessment of the vestibulo-ocular reflex (VOR). In the work of the vestibular system, the VOR is of utmost importance: thanks to it, a person can keep the object of observation in the field of view during various movements of the head. This is possible due to the fact that when the head is turned to the side, the eyes make a movement of the same amplitude and speed in the opposite direction.
VOR is assessed using the head rotation test (Halmagi-Kertoiz test): the patient is asked to fix his gaze on an object (for example, the doctor’s nose), then the doctor clasps his hands around the patient’s head in the temporal regions and sharply turns the patient’s head to the right and left by 10-20 °.
Normally, when turning the head, the gaze remains fixed on the object. The same thing is observed with damage to the central part of the vestibular analyzer. When the peripheral part is affected, when the head is turned, the eyes first move in the direction of the turn, after which the gaze is again fixed on the object.
Marching test (Fukuda test). To carry out the test, the patient closes his eyes, stretches his arms forward and begins to walk in place, raising his knees high. After 50 steps, the doctor assesses how much the patient has deviated from the initial position; normally, the angle of deviation should not exceed 30-45°. If there is a unilateral peripheral lesion, the patient turns towards the affected labyrinth. In case of damage to the central department, there is a lack of coordination, deviation in different directions, sometimes the patient falls or turns towards the pathological process when the cerebellum is damaged [28].
Postural reflexes , which make it possible to maintain a stable body position, are examined by gently pushing the patient into the upper torso. At the same time, the doctor is behind his back so that the patient does not see when and in what direction he will be pushed. With vestibular disorders, instability is possible, but in general the person maintains the posture.
Gait assessment (with eyes open and then closed). When observing a patient's gait, a balance disorder is often diagnosed. Many diseases of the peripheral and central nervous system are accompanied by typical gait changes, but in most patients with vestibular disorders it is not impaired, except in the acute stage of the disease.
An orthostatic test involves measuring blood pressure while lying down, immediately after moving to an upright position, and then over the next three minutes. The test is considered positive if systolic blood pressure decreases by 20 mmHg. Art. or more or diastolic pressure decreases by 10 mm Hg. Art. and more. The method allows you to identify pre-fainting conditions associated with orthostatic hypertension.
Instrumental examination
In most cases, data from a detailed survey, analysis of complaints and examination of the patient are sufficient to make a diagnosis. Instrumental methods are necessary if a central lesion of the vestibular analyzer is suspected and in the presence of concomitant diseases (for example, previous acute cerebrovascular accidents, the presence of space-occupying lesions or vascular anomalies in the past or present).
The need for computed or magnetic resonance imaging (CT/MRI) may arise if objective data are detected that require further examination. For example, vertical nystagmus, multidirectional, beating down or up may indicate damage to the stem structures of the brain or cerebellum [1].
Most often, CT and MRI can diagnose cerebral infarction, cerebral hemorrhage, multiple sclerosis, tumors of the brain stem and cerebellopontine angle, anomalies and other diseases accompanied by dizziness.
Ultrasound examination of extracranial and intracranial arteries is indicated if cerebrovascular disease is suspected with an appropriate history and the presence of risk factors (arterial hypertension, diabetes mellitus, obesity, hypercholesterolemia, heredity for cardiovascular diseases, previous acute cardiovascular diseases).
For dizziness that is accompanied by noise in the ear or hearing loss, pure tone threshold audiometry to determine auditory sensitivity to sounds of different frequencies. During this examination, the auditory threshold of bone and air conduction is compared, and if deviations from the norm are detected, the probable cause is determined (cerumen plug, otosclerosis, labyrinthitis, Meniere's disease, etc.).
A cardiac examination (ECG, ECHO-CG, Holter monitoring) is indicated if a cardiogenic cause of dizziness is suspected [5][8].
Stabilography is the study of balance using a moving platform. Using this method, it is possible to quantify involuntary postural reflexes, thanks to which a person does not fall, and also determine what role information from various senses plays in maintaining balance.
Questions and answers
At what age does amnesia most often occur?
Typically, amnestic syndrome appears in people after 65 years of age due to senile changes in the brain. In other age groups, amnesia can occur after trauma, severe intoxication, or as a result of severe psycho-emotional shocks.
Is it possible to restore memory without taking medications?
Even with a regressing form of the disease of organic origin, certain groups of drugs may be required to restore memory in full. They will help normalize metabolic processes and restore bioelectric impulses. If amnesia appears after stress, then in mild cases, competent psychotherapy will be sufficient.
Losing your balance in the dark
There may be cases of loss of balance in the dark. The disorder may occur due to chronic vestibular dysfunction. Increased symptoms in the dark are due to the fact that in such a situation vision cannot compensate for the defect. As a result, simply going to fetch water at night will cause significant difficulty and often end in a fall. Loss of balance in the dark is caused by drug intoxication, damage to the cerebellum, and disorders in the cervical spine. If the cerebellum is damaged, visual control is not important and the person will constantly experience a feeling of loss of balance.
Unsystematic sudden dizziness
About 30% of complaints about dizziness and loss of balance are called false, that is, non-systemic. The sensations are not associated with the development of the disease and can occur in the following situations:
- a sharp change in body position when standing up after prolonged sitting or lying, a sharp turn of the head. The feeling of loss of balance lasts seconds and is associated with the redistribution of blood in the vessels;
- the appearance of feelings of fear or anxiety. Dizziness is caused by a psychological factor;
- overwork, lack of sleep;
- lack of nutrients during an irrational diet;
- dizziness during pregnancy may be associated with the development of anemia, fatigue, changes in the body during pregnancy;
- intoxication with medicinal, alcoholic and narcotic substances causes a feeling of loss of balance and dizziness due to the toxic effect on the vestibular apparatus.
Where to go and which doctor
If you experience constant dizziness and a feeling of loss of balance, you should seek help from a neurologist. The doctor will determine the reasons for the development of this condition and prescribe the necessary treatment. If during the diagnostic process it turns out that the cause of dizziness and loss of balance is not a neurological disease, the doctor will refer the patient to the appropriate specialist (cardiologist, otolaryngologist, etc.) to eliminate the problem.
The Yusupov Hospital is equipped with the latest technology. The latest equipment from global manufacturers is used here. This allows you to diagnose any disease quickly and in the shortest possible time. Timely diagnosis greatly facilitates the treatment process and eliminates possible complications and unpleasant consequences.
The Yusupov Hospital is located near the center of Moscow and receives patients around the clock. You can make an appointment and get advice from specialists by phone.