Catatonia is a psychopathological syndrome with a predominance of psychomotor and autonomic disorders in the motor sphere, characterized by a clinical picture of agitation or stupor, which is unmotivated.
In the International Classification of Diseases (ICD-10), the disorder is considered within the framework of catatonic schizophrenia. This interpretation makes it difficult to diagnose the disorder.
Catatonic states of excitement and stupor can quickly replace each other. They arise autochthonously and are functional in nature. Catatonia may not be accompanied by stupefaction (lucid), or may be accompanied by oneiric stupefaction.
Catatonic stupor is characterized by increased muscle tone and immobility. Stupor can develop quickly or gradually. With gradual development, slowness, angular movements, prolonged freezing in one place (substupor), etc. initially appear. Over time, the severity of stupor increases.
Variants of motor stupor:
- Depressive;
- Catatonic;
- Hallucinatory;
- Apathetic;
- dissociative (“hysterical”);
- affective-shock.
Types of motor excitation:
- Manic;
- Anxious;
- Hallucinatory;
- Delusional;
- Affective-shock;
- Dissociative (“hysterical”);
- Against the background of confusion: delirium, twilight confusion.
Catatonic excitation develops suddenly, often rapidly moving from a state of stupor.
Catatonia is also characterized by other clinical manifestations:
Mutism is an unmotivated refusal to speak during normal functioning of the speech apparatus. Passive and active negativism is an unmotivated refusal to perform actions (for example, changing a position) or performing opposite actions. Motor and speech stereotypies - pretentiousness of movements and facial expressions. Echopraxia and echolalia are unmotivated repetition of the actions and phrases of others.
Causes
Specific reasons for the development of catatonia have not been established. The disorder may be initiated due to:
- Concomitant mental disorders (depression, bipolar disorder, schizophrenia, schizotypal disorder, acute psychosis);
- Substance and alcohol use;
- Neurological diseases (epilepsy, multiple sclerosis, Parkinson's disease, brain tumors, dementia);
- Metabolic and endocrine disorders (Cushing's syndrome, hyperthyroidism, Sheehan's syndrome);
- Autoimmune diseases (systemic lupus erythematosus, antiphospholipid syndrome), etc.
Genetic predisposition to certain mental disorders plays a great role. Some infectious diseases can also cause the development of catatonic stupor.
Diagnosis of catatonia
During the diagnostic process, the psychiatrist needs to identify the symptoms of catatonia and determine the underlying pathology that provoked the development of catatonic syndrome. If schizophrenia, depression or mania is suspected, the doctor obtains medical history from the patient’s relatives. While maintaining contact, the psychiatrist talks with the patient to identify productive symptoms. If contact is impossible, the presence of delusions and hallucinations is established indirectly, taking into account the patient’s behavior. All patients undergo a neurological examination.
To make a diagnosis of catatonic schizophrenia, at least one of the following symptoms must be present for 2 weeks:
- Catatonic agitation;
- Catatonic stupor;
- Any kind of negativism;
- Catalepsy;
- Waxy flexibility;
- Rigidity and automatic obedience to the instructions of medical personnel.
To diagnose depression or mania with psychotic symptoms, the presence of stupor is sufficient; other signs are not necessary.
Intoxication and post-intoxication states are identified on the basis of anamnesis (registration for drug addiction, treatment in a drug treatment clinic), the words of relatives and objective signs of psychoactive substance use. If organic pathology of the brain is suspected (malignant and benign neoplasms, head injury, vascular diseases), consultations with relevant specialists are prescribed: neurologist, neurosurgeon, oncologist, etc. The scope of additional research is determined by the identified pathology.
The mandatory list of tests includes a complete blood count, biochemical blood test, urine drug test, blood sugar level determination and thyroid hormone level determination. Depending on the results of the examination, CT and MRI of the brain, electroencephalography, ECG, spinal puncture, blood serum testing for antibodies, tests for HIV and syphilis, blood and urine culture may be prescribed.
If you notice at least one symptom in yourself or your relatives, consult a doctor immediately. The best doctors at the Yusupov Hospital will conduct an examination, study external signs and provide the necessary assistance. Yusupov Hospital is open for you around the clock. If you have previously performed any tests, be sure to take their results to a consultation with your doctor. If tests have not been performed, they can be performed directly at the hospital.
Pathogenesis
There is no consensus on the pathogenesis of catatonia. Studies have shown that disruption of communication between cortical structures, the thalamus and the basal ganglia play an important role in the occurrence of catatonic symptoms, therefore, in addition to clinical assessment, when studying catatonia, it is worth taking into account the results of neuroimaging and neuropsychological examinations. The hypothesis is based on a lack of gamma-aminobutyric acid (GABA) in the basal ganglia. Normally, GABA reduces the intensity of emotional reactions, such as anger, fear or anxiety.
In modern literature, there are often cases of catatonia caused by abrupt withdrawal of drugs used to treat catatonic states and accompanying mental disorders. This therapy uses mechanisms to increase GABA activity in the basal ganglia, which has a positive therapeutic effect. With abrupt withdrawal of drugs, an increase in motor symptoms often occurs (the phenomenon of “rebound catatonia”).
It is possible that catatonia develops as a result of severe anxiety, in response to stress. Therefore, scientists suggest that catatonic states are directly related to affective and other mental disorders that are accompanied by symptoms of severe anxiety.
Treatment
Treatment of catatonic syndrome is a difficult process, this is due to the polyetiological origin of the pathological process, as well as the fact that it can be provoked by certain types of substances. Often, for this disorder, drugs of the benzodiazepine group are used, in particular Lorazepam, Phenazepam, Nozepam, Gidazepas, Dorozepam. Severe forms of catatonic syndrome are indicative of ECT, and the voltage of the effect is correctly selected with the help of a good specialist. The procedure itself, if done correctly, is not very traumatic, but can produce remission for a long time.
A gentle approach is important with antipsychotic drugs due to the possible worsening of catatonic symptoms. In addition, the disorder has a tendency to worsen if it is not treated correctly. The neuroleptic, which was developed for catatonic symptoms, Mazeptil, has an excellent effect, but is difficult to obtain in pharmacy production.
Patients with catatonic syndrome are more prone to neuroleptic syndrome due to the presence of organic lesions in the brain; this pathology is deadly. That is why it makes sense for such individuals to prescribe all dosages at the lowest possible dose. Neuroleptics are indicated for treatment-resistant catatonic syndrome: Soleron, Adagio, Rispaxol, Eglonil, Olanzapine.
Effective in some forms of disorder, especially in the presence of affective inclusions - mood stabilizers. These include: Carbamazepine, Lithium carbonate, Lamotrigine, Lithium salt, Valprocom. In some cases, sleeping pills are used: Zolpidem, Zolpiclone. Often, especially in combination with dementia, it is important to use NMDA receptor antagonists: Memox, Mema, Memantine, Amantadine.
For the correct application of therapeutic approaches, it is important to exclude the presence of concomitant neurological and even somatic disorders, which can significantly affect the course of the disease. Often, with the stuporous form of the disease, intensive care observation is necessary, since due to negativism and immobilization, the patient does not feed on his own and may die from hunger and disease
Often, even tube feeding is not enough and resuscitators switch to parenteral administration of all necessary fluids and nutrients.
For malignant neuroleptic syndrome, which masquerades as catatonic syndrome, muscle relaxants are used, for example, Sodium Datrolene. Dopamine agonists are also relevant: Bromocriptine.
Symptoms
There are many clinical signs of catatonic syndrome. Symptoms are often related to the motor area. With catatonic stupor, the patient becomes numb or completely immobile. Muscle tone is increased, especially in the head and shoulder girdle. The chewing muscles are toned, the lips are pulled forward (proboscis symptom), the person lies on his back, holding his head above the pillow (the “air cushion” symptom). Less severe conditions occur in the form of catalepsy. Muscle tone may alternate with complete relaxation, and epileptiform seizures are sometimes observed. The state of catatonic excitement is characterized by incoherent speech, absurd rhyming, and echolalia.
In severe cases, the attack of stupor with catalepsy is prolonged, mutism, lack of reaction of the pupils to intense painful stimuli (Bumke's symptom), and persistent insomnia are noted.
Stupor may be accompanied by oneiric stupefaction, delusions and hallucinations. Motor disturbances manifest themselves in combination with a feeling of stiffness of the body and the inability to move, with stupor, or a feeling of muscle looseness with motor excitement.
In catatonic states, the following symptoms may occur:
- catatonic stupor or substupor - complete or partial immobility, often in a sitting or standing position;
- catalepsy - a person remains in one position for a long time;
- waxy flexibility - long-term preservation of the position that another person gives the patient;
- negativism—resistance when another person tries to change the patient’s position;
- mutism – prolonged silence;
- stereotypy - repeated monotonous movements;
- catatonic agitation - increased disordered motor activity;
- echolalia/echopraxia - copying the words and movements of another person;
- pretentiousness of facial expressions and movements.
In addition to the main symptoms, manifestations of disruption of the autonomic nervous system may occur. With catatonia, there may be an increase in body temperature to subfebrile, a feeling of thirst, increased blood pressure, and tachycardia. Often patients refuse water and food.
The detailed picture of catatonic stupor and agitation does not differ in clinical manifestations in adolescents and adults. Oneiric catatonia often occurs against the background of the manic phase in schizoaffective psychosis; it is much less common in depression and attacks of fur-like schizophrenia, especially in adolescents. Hebephrenic syndrome is characteristic of adolescence and the malignant course of schizophrenia. As a rule, catatonic symptoms appear against the background of this syndrome.
Fibril catatonia develops with symptoms of oneiric, neurological and somatic disorders. A febrile attack is characterized by manic-delusional, hallucinatory and depressive syndromes. With more pronounced psychosis, fantastic delirium appears. The patient is in a state of agitation or stupor.
Body temperature rises sharply to febrile and higher. There is no relationship with somatic and infectious diseases. Blood pressure rises, tachycardia and increased sweating are present. The person is in an excited state and feels very thirsty. Excitement gives way to stupor or sub-stupor. General health worsens. The feeling of thirst and hunger disappears, the skin becomes dry, and swelling appears. If assistance is not provided in a timely manner, congestion in the lungs, bedsores and other complications may develop.
Most often, attacks of febrile catatonia are observed in people 41-50 years old. They are characterized by a severe course and a high risk of death.
With primary manifestations of catatonia, you should immediately consult a doctor. With timely diagnosis and effective treatment, the condition can be normalized without further development of complications.
PsyAndNeuro.ru
Catatonia is a psychomotor syndrome associated with a number of conditions encountered in psychiatry. Its manifestations range from stupor to agitation and include such pathognomonic features as verbigeration and waxy flexibility. The presence of volitional disorders in catatonia has led to the fact that for a long time it was considered as a subtype of schizophrenia, but currently we are talking about its high prevalence in mood disorders, combination with delirium and comorbidity with somatic pathology.
There is evidence that approximately a third of patients with delirium caused by a general medical condition in an acute state will develop catatonia during the period of hospitalization. In psychiatric services, the prevalence of catatonia varies from 1-6% to 8-9%. An accurate assessment of the prevalence and incidence of catatonia depends on the correct definition of its symptoms. Clinicians often mistake the signs of catatonia for something else or miss them altogether. It should also be remembered that one of the classic signs of catatonia is disorders of the autonomic nervous system (tachycardia, hypertension or fever), which do not occur in all patients.
The Bush-Francis Catatonia Rating Scale (BFCRS) and DSM-5 criteria can be used to identify catatonia, but the structure of catatonia remains unclear. Not many psychometric studies of the syndrome have been published, and most of them were devoted mainly to patients with psychotic disorders, and therefore are not fully representative. Wilson et al. looked at the presence of catatonia in 339 acute patients using the BFCRS. 232 individuals from this sample met the definition of confirmed catatonia (≥2 signs of catatonia on examination and a positive response to treatment with benzodiazepines or ECT). Of these, 211 (91%) met DSM-IV criteria for catatonia, but only 170 (73%) met DSM-5 criteria. When identifying the main components of catatonia, the following were identified: psychomotor agitation, psychomotor retardation and abnormalities of psychomotor behavior. Only 37% of the variability was explained, leading the authors to conclude that the underlying structure of catatonia remains unknown. Catatonia can be considered as a syndrome accompanied by motor disturbances, “paralysis of the will,” and fear.
Both volitional disorders and fear can lead to disturbances in the motor sphere, but most researchers have considered motor disorders as the main feature of catatonia. Many researchers have noted the similarities between catatonia and neurological movement disorders (including parkinsonism, dyskinesia and mild neurological signs). This can be explained both by the conceptual similarity between the rating scales used and by the presence of common pathogenic pathways. Depending on which scale is used, symptoms of catatonia can easily be missed or misinterpreted.
The similarities between catatonia and tonic immobility, which is a defensive strategy in fear in animals, have led to the hypothesis that catatonia is a primitive manifestation of fear. This hypothesis is supported by affective and neuroendocrine disorders in patients with melancholic depression and catatonic symptoms and the therapeutic effect of benzodiazepines. Imaging studies of the amygdala, ventromedial and dorsolateral prefrontal cortices may clarify this hypothesis.
The course and manifestation of acute catatonia in some cases resembles the course of encephalitis, which has led to the hypothesis that the cause of catatonia is a violation of immune regulation.
Catatonia is associated with disturbances in the motor cortex. As with Parkinson's disease, this syndrome involves hypo- and hyperkinesis, suggesting disturbances in more than one motor pathway. Three main pathways are thought to be involved during psychosis. One of them is responsible for motor inhibition and excitation and is a circuit from the primary motor cortex (M1) to the putamen, globus pallidus, thalamus and again to M1. The second pathway is responsible for the dynamics of movements and includes M1, thalamus, cerebellum and pontine nuclei. The third corticocortical pathway is thought to control the organization and speed of movements and includes M1, the supplementary motor area, the posterior parietal cortex, and the medial prefrontal cortex. Thus, according to this model, catatonic symptoms involving motor agitation or retardation would be associated with at least two of these three pathways.
Neuroimaging studies of patients with catatonia have shown low functional activity of the supplementary motor area, primary and secondary motor cortices, inferior parietal cortex, and basal ganglia during independent movements, decreased blood flow in the right prefrontal and parietal cortices, and decreased GABA-A receptor density in the left sensorimotor cortex. There is increased activity in premotor areas in individuals with hypokinetic catatonia. Increased thalamocortical activity (with M1) at rest was associated with increased BFCRS scores (i.e. observed in patients with more severe catatonic symptoms). The findings indicate the involvement of the motor system in catatonia. White matter may also be involved, although there is little direct evidence for it in patients with catatonia.
First-degree relatives of patients with catatonia are more likely to have mood disorders. The most common symptoms of catatonia, such as psychomotor retardation and agitation, showed a moderate degree of occurrence within families, whereas the classic symptoms, such as mutism or rigidity, showed a high degree of occurrence within families. The lifetime risk of catatonia in first-degree relatives of individuals with periodic catatonia is 27%, and there is an autosomal dominant association with chromosome 15q15 and a heterogeneous association with chromosome 22q13.
In individuals with schizophrenia who are heterozygous for cyclic nucleotide phosphodiesterase ( Cnp+/
–), after 40 years spontaneous catalepsy, apathy and social isolation develop.
It is known that the CNP
is more common in patients with schizophrenia and catatonic symptoms compared to patients without catatonic symptoms.
- Make a correct diagnosis of catatonia using rating scales or other diagnostic criteria.
- Prevention of venous thromboembolism, bedsores, contractures. Ensure adequate hydration and nutrition.
- For acute catatonia, benzodiazepines (lorazepam) are administered sublingually, intravenously or intramuscularly.
- In the absence of response to benzodiazepine therapy or in the case of a life-threatening condition, ECT is used.
Benzodiazepines and ECT are a safe and effective standard of care, especially for acute catatonia. Lorazepam, the benzodiazepine of choice for catatonia, is given sublingually, intravenously, or intramuscularly and is effective in both low (1–3 mg/day) and high (6–16 mg/day) doses. Although lorazepam is not effective for chronic catatonia in one randomized controlled trial, acute catatonia responds well to benzodiazepine therapy in 66% to 100% of cases. However, in a significant number of patients the response to benzodiazepines is insufficient - in 27% there is only a partial reduction of symptoms.
Treatment of patients with signs of both catatonia and delirium presents some difficulties. In particular, antipsychotics are currently the standard of care for delirium but may worsen catatonia, while benzodiazepines are first-line treatment for catatonia but may worsen delirium.
Some evidence suggests that patients with psychotic disorders and catatonic symptoms respond better to clozapine and low dopamine receptor affinity antipsychotics rather than to high dopamine receptor affinity antipsychotics.
Beach et al. A systematic review of alternative treatment strategies for catatonia concluded that intravenous lorazepam and ECT should remain first-line treatment. The authors suggest glutamate antagonists and anticonvulsants (carbamazepine and valproic acid) as second-line therapy if benzodiazepines and a full course of ECT are ineffective.
- Using Catatonia Rating Scales to Establish Symptom Severity in Various Conditions
- The use of resting neuroimaging for catatonia in various conditions, with specific symptoms, in acute and chronic conditions and longitudinally in individual cases
- Studying the dynamics of dysfunction of the autonomic nervous system in catatonia
- Organization of double-blind randomized controlled trials of treatment regimens for catatonia
- Development of an animal model of catatonia
The authors also believe that new non-invasive brain stimulation technologies are promising in terms of targeted effects on both local and distant disorders in the motor pathways, which opens up opportunities for individualized treatment of catatonia. It is necessary to study the effects of repetitive transcranial magnetic stimulation in various catatonic states
Future research should be aimed at clarifying the different types of manifestations, the course of the disease and the mechanisms of its development, while neuroimaging can help study neural networks and develop treatments.
Author of the translation: Lafi N.M.
Source: Sebastian Walther, Katharina Stegmayer, Jo Ellen Wilson, Prof Stephan Heckers. Structure and neural mechanisms of catatonia. The Lancet Psychiatry. Published: June 10, 2019 https://doi.org/10.1016/S2215-0366(18)30474-7
Classification
Catatonic states are classified based on the severity of clinical manifestations and the nature of the course of the disorder. Currently, there are two types of catatonia: benign and malignant. Malignant catatonia is the most severe form of the disorder and poses a threat to the patient’s life (“lethal” or “febrile” catatonia).
Febrile catatonia is an acute mental disorder accompanied by a deterioration in general physical condition: increased body temperature, somatovegetative disturbances, homeostasis disorders, deterioration in the functional ability of body systems. The condition develops without connection with somatic diseases. With such a course of the disorder, there is a possible risk of developing cerebral edema and multiple organ failure
Catatonia that occurs at the onset of the disease is considered primary (often observed in schizophrenia). If catatonic manifestations develop against the background of a prolonged course of the disease, catatonia is secondary.
Often in psychiatry, a classification of catatonia is used, based on the pattern of the underlying disorder and the predominance of catatonia syndrome over other symptoms. According to these signs, minor and extensive catatonia are distinguished.
Mild (small) catatonia
. is a reduced version of the catatonic syndrome, in which some simple manifestations are present. Negativism is not clearly expressed, substuporous states, short-term stops of movements and speech, episodic echolalia, isolated grimaces and unexpected actions are noted. The patient enters into dialogue only under duress, is reluctant to answer questions, his speech is mannered, and he avoids visual and tactile contact with the interlocutor. This condition is most often observed in developing schizophrenia.
According to the degree of severity, catatonic excitation is:
- ecstatic - patients are mobile, talk a lot;
- hebephrenic - ridiculous, inappropriate jokes, unmotivated and unreasonable gaiety predominate;
- impulsive - unexpected actions, often destructive and aggressive;
- silent - motor agitation with aggression and destructive actions.
Silent (mute) catatonic agitation
. The person makes meaningless, chaotic movements and resists other people’s attempts to help. During this period of arousal, there is a risk of harm to yourself and others.
Impulsive catatonic agitation
. Development is fast. A person copies the movements and phrases of nearby people. Speech is limited to a chaotic set of phrases. There is a tendency towards cruelty and destructive actions, and a high risk of self-injury.
Ecstatic
. Symptoms increase gradually. At the beginning, there is little motor and speech activity. The nature of the speech is mannered, echolalia (copying other people's words) is possible, and laughter often occurs for no apparent reason.
Degrees of severity of catatonic stupor:
Cataleptic
(with waxy flexibility). Muscle tone is increased, a person can maintain an uncomfortable position for a long time. Manifested by symptoms: catalepsy, waxy flexibility (maintains a position devoted to another person), “air cushion” (characteristic position on the back with the head raised above the pillow).
With negativism
. More pronounced muscle tension. There is sharp opposition to passive movements and attempts by other people to change the patient’s posture. Mutism is often observed.
Rigid
. Muscle tone is very pronounced. Due to the predominance of flexor muscle tone, the person is in the fetal position (knees brought to the stomach, hands pressed to the chest). Trying passive movements increases muscle tension. Muscle tone decreases during deep sleep.
Catatonic states are divided into two types - oneiric and lucid, depending on the presence of clouding of consciousness. With oneiric clouding of consciousness, ecstatic, impulsive, hebephrenic excitement, stupor with waxy flexibility and substuporous states develop. With lucid catatonia, stupor with negativism often develops.
Oneiric catatonia
combines a state of stupor and a dream-like state with vivid scene-like hallucinations, which the patient can talk about after emerging from the stupor. During stupor, the patient is most often disoriented and unable to perceive surrounding events; perception occurs in a distorted form with dream-like fantasies.
Lucid catatonia
represents a stupor without clouding of consciousness. The perception of what is happening around is not distorted. The patient is normally oriented in time and space, remembers the events that occurred while in a stuporous state. Sometimes partial amnesia occurs regarding one's own movements and behavior. The patient may not remember his own impulsive actions, prolonged immobility, etc.
Taking into account diagnostic approaches, catatonia is classified according to provoking factors:
Catatonia developed against the background of concomitant mental disorders. Most often, catatonic schizophrenia is considered (if motor disorders are the main clinical symptoms of the disorder), affective disorders with catatonic symptoms, and others.
Catatonia due to somatic illness. Catatonic syndrome may indicate neurological, infectious and other diseases with metabolic disorders.
Unspecified catatonia. Catatonic states without correlation with other mental and somatic disorders.
Symptoms of catatonia
With “empty” catatonia, the patient repeatedly reproduces the same poses (stereotypy), movements and phrases, repeats words and movements after other people (echopraxia). Active, passive or paradoxical negativism is observed. With active negativism, the patient does something that does not comply with the instructions; with passive negativism, he ignores any requirements; with paradoxical negativity, he does something opposite to the request. Catalepsy is detected - a condition in which the patient maintains one position for a long time or parts of his body freeze for a long time in any position, even an uncomfortable one.
With lucid and oneiric catatonia, the listed manifestations of the disease are supplemented by productive symptoms. In the lucid form of the disease, delusions, hallucinations and mood changes occur against the background of clear consciousness. With oneiric catatonia, disturbances of consciousness are observed. After recovering from catatonia, the patient partially or completely forgets what happened to him or in his presence, but retains fragmentary or detailed memories of the manifestations of the disease.
Catatonic excitation occurs continuously or is replaced by catatonic stupor. Catatonic stupor is manifested by a slowdown or almost complete disappearance of movements and an increase in muscle tone. With stupor, hyperhidrosis, hypersalivation, decreased blood pressure, swelling and cyanosis of the extremities often develop.
Complications
The development of complications is often associated with late diagnosis and incorrect approach to treating the disorder.
When treating people with severe forms of catatonia, difficulties may arise in the daily care of patients, as a result of which complications may develop:
- aspiration pneumonia - occurs due to the difficulty of eating in patients with mutism and the risk of aspiration;
- risk of deep vein thrombosis and pulmonary embolism due to immobility in people with catatonia;
- metabolic disorders associated with dehydration and exhaustion of the body - patients with catatonia may not eat or drink for a long time;
- disorders of the gastrointestinal tract (constipation, intestinal obstruction, etc.)
- urinary retention or incontinence;
- neuromuscular complications (flexion contracture, nerve palsy)
- formation of bedsores.
Also, in a state of catatonic excitement, the patient poses a danger to himself and others. The sudden onset of an attack of stupor can lead to an accident, overtaking a person driving a car, while crossing the road, at work, etc.
Complications of severe forms of catatonia are difficult to treat due to the difficulties in contact between the patient and the doctor.
Treatment
Even among doctors, there is an opinion that it is impossible to remove a person from a state of catatonic stupor so that he does not experience it in the future. It would be logical to decide that there is no main treatment to completely eliminate the disease.
However, scientists are constantly conducting various studies and tests, which today can already say the opposite. If the diagnosis is made on time and treatment is started immediately, you can count on remission. There are several drugs that have been continually researched and used for patients with catatonia. As a result, good results were revealed. In particular, among these drugs:
- carbamazepine, which is a kind of mood stabilizer;
- benzodiazepine;
- antipsychotropic drugs;
- dopamine antagonists, which help improve production and NMDA antagonists;
- muscle relaxants.
To ensure that the drug is truly beneficial, many experts strongly recommend the use of additional treatment methods. In particular, this is the use of electroconvulsive therapy through electric shock. Treatment may not always show positive results. Sometimes side effects may occur.
In particular:
- strong aggression, which leads to injuries with elements of suicide;
- complete refusal to eat;
- development of neuroleptic malignant syndrome;
- development of pulmonary embolism.
According to statistics, about 40% of patients can be conditionally called curable. About 70% of patients also show significant improvements after taking a benzodiazepine. All these indicators indicate that the pathology in question is not a death sentence, since modern medical treatment methods are constantly evolving, the main thing is to see a doctor in time.
Diagnostics
When diagnosing catatonic states, it is important to correctly assess the patient’s clinical condition. When collecting anamnesis and examination, it often turns out that the person used psychoactive substances, which most likely contributed to the development of catatonic syndrome. It is worth considering the likelihood of developing symptoms of catatonia during treatment with psychotropic drugs for concomitant diseases.
Psychometric scales are used to diagnose the disorder. The most commonly used is the Bush-Francis Catatonic Disorder Scale. It allows you to determine the presence and severity of catatonic symptoms over a certain period of time. Other rating scales are also used.
Electroencephalography (EEG), CT, MRI and neuropsychological examinations allow us to suggest the localization of disorders in the brain and diagnose the functional state of higher mental functions.
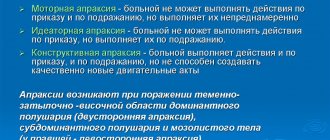
Differential diagnosis is carried out with other mental and somatic disorders accompanied by motor disorders. The most clinically similar to the catatonic syndrome is Parkinson's disease, but the disease is accompanied by a number of specific symptoms that make it possible to differentiate it from catatonia (tremor, apraxia of walking).
Catatonia is differentiated from schizophrenic catatonia, acute psychoses with motor agitation, conversion disorders and other conditions with severe motor retardation or agitation, and neurological symptoms.
Catatonic state: general description
The syndrome was first described at the end of the 19th century by the German psychiatrist K. Kahlbaum, and for a long time it was considered as a separate disease, and doctors noted that even despite intensive treatment, there is a high probability of an unfavorable, progressive course. At the beginning of the 20th century, catatonic disorders were described exclusively as one of the typical symptoms of schizophrenia, and only in the early 2000s was the connection of such a disorder not only with other mental, but also with somatic diseases established and proven.
What is “catatonia” in simple words? The pathology is accompanied by severe movement disorders from complete immobility to acute agitation. At the same time, patients do not react at all to speech addressed to them and aggressively perceive attempts to calm them down.
The pathogenetic mechanisms of the occurrence of catatonic symptoms are not completely known today. There are several hypotheses for its development:
- disturbances in the production and metabolism of neurotransmitters, mainly γ-aminobutyric acid, and to a lesser extent, dopamine;
- organic lesions of individual foci of the brain, in particular, the orbitofrontal cortex, basal ganglia;
- neuroendocrine changes caused by pheochromocytoma, thyrotoxicoma, hypoparathyroidism (however, endocrinopathies are only one of the provoking factors in the development of affective catatonic syndrome);
- an autoimmune inflammatory process affecting the central nervous system.
Forecast
Mild forms of catatonia usually do not have a strong impact on the patient’s further social adaptation and respond well to treatment. Treatment is carried out in a psychiatric hospital. In case of severe somatic diseases, hospitalization is carried out in a specialized department (neurological, oncological). A poor prognosis is associated with catatonia of a malignant course, due to the risk of death, and the presence of catatonia in children, adolescents and the elderly with schizophrenia. Such people require constant psychiatric treatment. Relapses of catatonic states most often occur with the idiopathic version of the disorder or in the presence of concomitant affective disorders. If a person has renal failure, Parkinson's disease, or alcohol addiction, the dysfunction of the brain is chronic, which can also lead to relapses.
In most cases, the prognosis of catatonic syndrome depends on the course of the underlying disease and timely treatment.
Causes of catatonic disorders
Catatonia has not yet been thoroughly studied by doctors. Therefore, it is impossible to say exactly what processes cause the disease. At the same time, experts do not exclude the influence of a hereditary factor on the occurrence of pathology. Signs of catatonic syndrome are observed in individuals who suffer from a functional disorder of subcortical glutamatergic and cortical connections. They are also diagnosed with a malfunction in the balance of inhibition and excitation, blockade of dopamine receptors.
The disease is caused by congenital anomalies and obstetric pathologies. Doctors include organic disorders that are caused by intoxication of the body and injuries as a group of causes. The risk group includes people who are exposed to the following negative factors:
- Hysterical neurosis;
- Postpartum psychosis;
- Autistic disorder;
- Epilepsy;
- Traumatic brain injuries;
- Stroke;
- Tourette's disease;
- Congenital and acquired pathologies of metabolic processes;
- Autoimmune and endocrine pathologies of a chronic nature;
- Early amaurotic idiocy;
- Intoxication with narcotic substances.
Overuse of medications that are taken for a long time without medical supervision can also lead to catatonia.
Treatment in Re-Alt
When treating catatonia that has developed against the background of another mental or physical disorder, therapy is aimed mainly at the underlying disease. Therefore, it is very important for the effectiveness of treatment to conduct a thorough diagnosis. At the Re-Alt mental health center, specialists conduct a detailed analysis of each clinical case and assess the patient’s mental and somatic status in order to individually select treatment tactics.
The most effective method of treating catatonia is the use of drugs from the group of benzodiazepine tranquilizers. Pharmacotherapy helps reduce muscle tone and eliminate other manifestations of catatonia. Treatment uses drugs with sedative, anticonvulsant effects, and muscle relaxants.
If drug treatment is ineffective, electroconvulsive therapy may be prescribed.
Febrile catatonia is a medical emergency. Treatment is carried out inpatiently. Measures are prescribed to maintain and normalize the functioning of all body systems. Antibacterial therapy is prescribed to prevent complications. After stabilization of the condition, electroconvulsive therapy is performed
Treatment of catatonia
Before prescribing treatment for catatonia, it is necessary to conduct a thorough diagnosis and a comprehensive examination in order to exclude somatic and neurological causes that require appropriate treatment.
It is also recommended to conduct laboratory tests, such as blood and urine tests for drug content, electroencephalography and computed tomography. The results of most diagnostic tests indicate that only one patient out of ten suffers from catatonic stupor due to schizophrenia. In other patients, stupor develops due to affective disorders, most often due to various forms of mania.
The causes of catatonia can also be hidden behind deep depression. In addition, catatonic syndrome can be a consequence of postpartum mental pathologies and traumatic brain injuries. Also, the disease in question is often accompanied by temporal lobe epilepsy, severe forms of dementia, some somatic pathologies or infectious diseases.
Diagnosis of catatonic syndrome presupposes that the patient has clearly demonstrated one of the following signs of catatonia for fourteen days: stage of stupor, catatonic excitation, freezing in various positions, rigidity, negativism, waxy flexibility and automatic obedience (command automatism).
The fundamental strategy in the treatment of catatonic syndrome, regardless of its etiology and symptoms, is the prescription of benzodiazepine drugs (in particular Lorazepam) and the use of electroconvulsive therapy.
In the treatment of catatonic syndrome, the prescription of neuroleptics is not practiced, even if the pathology is caused by a psychotic disorder, since these drugs increase the risk of developing neuroleptic malignant syndrome and increase the likelihood of death. However, they can still be effective for therapeutically insensitive catatonia.
Mood stabilizers (Lithium) and NMDA receptor antagonists (Amantadine) are also considered effective for catatonic syndrome.
In addition to benzodiazepine drugs and electroconvulsive therapy for pathologies such as neuroleptic malignant syndrome, dopamine receptor agonists (for example, Bromocriptine) and muscle relaxants (for example, Dantrolene sodium) are recommended.
Some scientists are convinced that Carbamazepine (an antiepileptic drug belonging to the group of carboxamide derivatives) is effective in the strategy of both emergency first-line therapy and at the stage of maintenance treatment of catatonic syndrome. A study in which nine patients were treated with carbamazepine showed that four patients responded completely to treatment, one responded partially, and the remaining four patients did not show any productive changes.
A combination of an antipsychotic and lithium may be an alternative in the treatment of therapeutically insensitive catatonic stupor.
Treatment of one patient with resistance to benzodiazepines and electroconvulsive therapy showed the effectiveness of Zolpidem (a hypnotic drug belonging to the group of imidazopyridines).
Thus, conditionally treatment tactics can be divided into two groups: pharmacological agents, the effectiveness of which has been proven, and additional therapeutic measures. The first includes the following medicinal substances:
- benzodiazepine drugs (Diazepam);
— mood stabilizers or mood stabilizers (Carbamazepine, Valproic acid);
- antipsychotic drugs (Haloperidol);
- NMDA receptor antagonists (Memantine);
— muscle relaxants (Dantrolene);
- dopamine agonists (Bromocriptine).
The second group includes electroconvulsive therapy (electric shock).
We are on Telegram! Subscribe and be the first to know about new publications!