Medical information is reliable Checked by Eremin Alexey Valentinovich
Passive-aggressive personality disorder is a mental disorder that is accompanied by psychological resistance to external demands. Without treatment, the condition can lead to antisocial behavior, dismissal from work, and destruction of family ties and business contacts.
Therapy is based on individual or group psychotherapeutic sessions. In severe cases, drug therapy is used. Dr. Isaev’s psychiatric clinic offers treatment for passive-aggressive disorder in Moscow. Traditional approaches to psychocorrection and innovative developments of scientists are used here.
General information about the disease
Social conflicts and communication difficulties can occur in any person. They do not indicate any personality deviations. But in some cases these manifestations become pathological. Passive-aggressive personality disorder is characterized by the following features:
- a person tends to think in a negative way, he is pessimistic, gloomy, set up for failure;
- there is a belief that people around him are negatively opposed to him;
- the patient denies his own role in certain circumstances where he is guilty, tends to refer only to external factors;
- he has a fear of disapproval of his own words and actions from society;
- the patient is convinced that his personal freedom is being limited, and often considers himself offended and insulted.
To assert themselves, people with passive-aggressive personality disorder tend to assert their rights through irritation and aggression. At the same time, they may not express their dissatisfaction for a long time, hiding it from others.
Diagnosis of impulsive disorder in medical
The diagnosis is made based on generally accepted diagnostic criteria:
- tendency to rash, impulsive actions;
- tendency to groundless quarrels and conflicts;
- attacks of uncontrollable explosive behavior;
- emotional lability.
Special psychological tests are used to rule out other types of personality disorders. According to indications, a comprehensive examination is carried out to identify possible neurological pathologies (epilepsy, tumors, hematomas, thrombosis of cerebral vessels).
Causes of the disorder
Experts believe that a negative example of such behavior in parents becomes a serious risk factor in the development of passive-aggressive disorder in a child. Other reasons may be:
- chronic stress arising from conflicts in the family and at work;
- the emergence of transference and identifications. A person can identify with an aggressive person due to strong emotions, transferring to himself the character traits of a complete stranger;
- upbringing with authoritarianism, total control, overprotection.
Passive aggression is provoked by constant demands from parents to contain emotions. As a result of this, a person is unable to express them and can translate feelings into aggression towards other people. Very often, outwardly pleasant and reserved people, brought up in this way, are internally overstrained, filled with the desire to restore a certain justice to them alone.
Causes of the disease
There is a genetic predisposition, since emotional-impulsive disorder often occurs among blood relatives of patients. But burdened heredity alone is not enough to manifest the clinical manifestations of the syndrome. Many other factors are also involved in the pathogenesis of the disease.
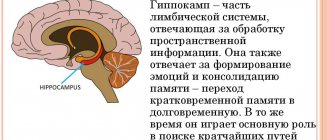
First of all, this is organic damage to the brain, especially the limbic system, which is “responsible” for the emotional background, motivation, and behavioral reactions. Considering that symptoms usually appear during puberty, the causes of the disease may be traumatic brain injury, previous encephalitis or other neuroinfections, or seizures in early or infancy.
In addition, factors that influence the intrauterine development of the central nervous system also play a certain role. This:
- use of alcohol, drugs, teratogenic drugs by the expectant mother;
- hypoxia of the placenta;
- poor nutrition of a woman, deficiency of essential vitamins and minerals due to malnutrition or pathology of the gastrointestinal tract;
- past viral infections.
The effects of these factors are especially dangerous in the first trimester of pregnancy, when the formation of the main structures of the brain occurs.
Not least important is the unfavorable psychological atmosphere in which children are raised. The risk of the syndrome increases many times over with alcoholism or drug addiction of the father and/or mother, coldness or vice versa, overprotection, lack of interest in the child’s problems.
Symptoms of Passive-Aggressive Personality Disorder
Passive-aggressive disorder is easy to recognize in everyday life. It manifests itself in the following acts of behavior:
- frequent complaints about loved ones, friends, colleagues;
- writing reviews in the book of complaints and suggestions in the absence of objective reasons;
- drawing up reports to superiors, which highlight the guilt of employees, because of which the patient considers himself to be a victim.
People with this disorder are characterized by the appearance of automatic thoughts and ideas that are negative in nature. Patients always choose the path of least resistance and move away from their colleagues around them. They negatively interpret any events in life and extend negativism to all their behavior.
They follow the path of minimal resistance - they put things off until later, do them poorly, with a long delay. In any difficulties, a person expresses his dissatisfaction with his boss and other people in power. As a rule, outbursts of anger occur rarely. Most often, dissatisfaction manifests itself passively. People sabotage activities and subtly persuade others to do the same.
The predominant emotions in a person with passive-aggressive personality disorder are anger and irritation. They arise from a constant feeling of being undervalued. At the same time, the person himself cannot achieve professional and personal goals, which confirms his feelings. Patients do not understand that their attitudes lead to this. They do not feel responsible for personal failures.
Basic clinical strategies
Often, when patients with personality disorders come for treatment, they are not interested in changing their existing patterns of thinking and behavior. Instead, they come to treatment because of a diagnosis, such as depression, or at the urging of others. This is especially true for people with PPD, as they are likely to believe that their difficulties are caused by others rather than by themselves. Therefore, treatment will initially focus on identifying the purpose for which patients came for treatment.
The first general approach when working with passive-aggressive patients is to focus on collaborative practice, that is, active participation in the psychotherapeutic process (Beck, 1976). Although this is a central component of cognitive psychotherapy in general, it is especially important when working with passive-aggressive patients, as they do not pay attention to people in authority. Therefore, it is important that they understand that they make their own treatment decisions and that the therapist is not directing or manipulating them.
The therapist may initially offer them a choice of several homework assignments or problems to discuss in session. Later, patients are encouraged to develop their own problem-solving strategies. It is helpful to work by tapping into patients' desire for autonomy while challenging their typically passive approach. This collaboration may also facilitate the use of an experimental approach. For example, if a patient strongly believes in his automatic thoughts or assumptions, it is better if the therapist does not try to discuss their correctness, but instead suggests that they be considered as hypotheses that may or may not be true. Then the therapist and patient can jointly come up with some kind of “experiment” to test their validity.
A second strategy with passive-aggressive patients is to help them get in touch with their automatic thoughts. Their lack of understanding indicates that they rarely think about how cognitive structures influence their emotions and behavior. This very general strategy will be the most important in the treatment program, and significant time should be spent early in treatment establishing the rationale behind the cognitive model. By becoming more aware of their thoughts, patients will learn to identify those automatic thoughts that cause negative emotions and dysfunctional behavior. Finally, of course, they must learn to evaluate these thoughts more objectively.
Another important general strategy is for the therapist to be consistent in treatment. The rules that are set regarding time, payment, etc. must be consistently followed. Since these patients blame others for their problems, this arrangement will help demonstrate that patients' attitudes and behaviors often lead to negative consequences. For example, if a patient is late for a session (which often happens with this type of patient), the therapist should end the session at the usual time. When such behavior is noted, the therapist can obtain feedback from the patient to determine whether this is a common passive-aggressive reaction to psychotherapy or the therapist.
The patient may have the following automatic thought: “I don’t have to get there on time, no one will tell me what to do.” Through discussion, the therapist can help the patient learn direct rather than indirect means of expression. For example, if a client does not want to schedule a session at a certain hour, he can tell the therapist that this time is undesirable or inconvenient. It may take several days before these patients are able to explore how their attitudes and behavior contribute to their difficulties, but this approach provides a basis for doing so.
The next important component of treatment is helping patients with PPD explore their methods of getting revenge on people. For example, if a patient is angry with someone and reacts by not doing a good job, beliefs such as “People should be punished” or “I will do what I want” should be explored. The advantages and disadvantages of such a strategy should be considered and alternative strategies should be developed. For this purpose, it is necessary to consider the sequence of events that occur in interactions with other people. Despite the obvious disadvantages of being negative towards others and being unpredictable, there are some benefits to these behaviors that otherwise would not persist. For example, with experiences of poor performance and unpredictability, passive-aggressive patients may find that they are less likely to be asked to perform certain undesirable tasks. (Paradoxically, this often causes resentment because patients may think that others are trying to control them in this way.) The therapist and patient need to consider these “positive” results so that the patient can not only see the consequences of this behavior, but also have motivation to use alternative methods of response.
A general strategy of encouraging patients to demonstrate appropriate social skills is also helpful. For those patients who lack social skills, the therapist should gradually teach these skills. When cognitive structures interfere with available appropriate social behavior, changes in specific cognitive structures are necessary.
Individual methods
Within these general strategies, a variety of specific techniques can be used to change the cognitive structures, emotions, and behavior of passive-aggressive patients. To help them identify automatic thoughts, you can first try the same steps that are used with most patients: in session, identifying automatic thoughts during emotional shifts and giving homework to identify other automatic thoughts that appear between sessions. For example, one patient felt irritated during a session and reported the thought: “I shouldn’t do anything. You are trying to dominate me." Because these patients are resistant to requests or demands and are interested in taking the path of least resistance, they are expected to be reluctant to identify automatic thoughts.
At this point, the therapist and patient should work together to identify which cognitive structures may be preventing the patient from completing the task. There are usually two types of such cognitive structures: the first produces negative emotions (e.g., depression and irritation), and the second consists of cognitive structures regarding reactions to “demands” (e.g., “I have to do this my way,” “Why do others always are they forcing me to do something?”, “It’s easier to do nothing and let everything work itself out”). Once these cognitive structures are identified, the therapist and patient can evaluate whether there is evidence that these conclusions or interpretations are valid and whether there are alternative and more valid explanations. If it is determined that the interpretation is not distorted, the therapist and patient should discuss the actual consequences, as well as strategies for solving the problem. For example, a patient may feel sad when he thinks, “Everyone at work hates me, and I'm doing a bad job.” The idea that everyone hates this person is probably an over-generalization; therefore, the therapist can help the patient question it by presenting facts that contradict it. At the same time, the thought about the poor quality of work may be correct. It is therefore useful to assess how poorly the patient is performing, what cognitive and motivational factors contribute to poor performance, and how the patient can change these factors.
Passive-aggressive patients may respond to questions about evidence for the validity of their beliefs by saying, “Because I feel it.” In these patients, such “emotional reasoning” often arises unexpectedly and must be confronted. For example, a patient might carry a card with them that says “Feelings are not facts” to remind themselves that emotional states are based on an interpretation of a situation and are not necessarily true. It is also useful to work with examples of such situations from the past of patients, when they made some conclusions based on their “feelings”, and then discovered that they were wrong.
When giving a passive-aggressive patient the task of recording automatic thoughts for the first time, it can be said that this is a “win-win” task. If the patient completes this, it will help to see which automatic thoughts contribute to anxiety and depression. If the patient does not complete it, it will be possible to identify cognitive structures that prevent the task from being completed. For example, one patient did not complete the task of recording automatic thoughts. She thought about this several times during the week, but each time she had the following thought: “Why bother? No one will force me to do what I don't want to do. I just don’t think it would be helpful, so I don’t do it.”
When working with these patients, specific cognitive psychotherapy techniques that promote collaborative relationships will be important. At the beginning of each session, the therapist and patient should jointly plan the structure and content of the session. Feedback should be asked at the end of each session and after certain interventions. This should be done to ensure that the patient understands the meaning of the procedures and also to become aware of any negative cognitive structures that he may have about the therapist or psychotherapy. As noted earlier, "experiments" can be conducted to test the validity of some of the cognitive structures that the patient has.
It may be useful to conduct a cost-benefit analysis of behavior. For example, if a patient does not agree to an appointment during work hours because he or she has thoughts of “I shouldn't do this” or “The appointment is at an inconvenient time,” the patient may believe that the benefit of not going to the appointment is in an indirect expression of his dissatisfaction with the “unfairness” of the situation. A cost-benefit analysis, however, may reveal that missing a meeting has negative consequences. The therapist and patient can then discuss ways in which the patient can express dissatisfaction more directly so that its absence is not misinterpreted.
Once the patient realizes that his strategies are not conveying messages accurately, it is important to develop assertiveness skills. Sometimes passive-aggressive patients have an effective alternative response in their repertoire, but do not use it because of dysfunctional assumptions. But more often these patients have deficits in response skills. In such cases, possible alternative responses can be discussed and role-played in sessions and then practiced during homework.
Relapse Prevention
One of the best strategies to prevent relapse is to provide support sessions. As with other personality disorder patients, BPPD patients' deep-seated dysfunctional beliefs may not become apparent until patients are exposed to a situation that activates them. Before completing psychotherapy, situations to which patients are vulnerable can be identified. As noted above, they can keep a “workbook” of these situations that includes typical automatic dysfunctional patterns as well as more rational and functional cognitive structures and behaviors. Examples of such situations include being treated unfairly, being told to do something, or evaluating a negative situation. Supportive sessions help prevent patients from reoccurring in dysfunctional patterns. These sessions can review successful strategies, discuss problem areas, and look for potential problems. During treatment, it is necessary to explain to the patient that psychotherapy is a way to learn how to effectively cope with various situations. It is quite natural that when stressful situations arise, the patient will have to use psychotherapy as a means of getting out of them.
Problems of a psychotherapist
It is not surprising that patients with PPD are difficult to work with because of their negativistic attitudes and frequent reluctance to use alternative approaches to problem solving. In addition, a passive-aggressive patient will inevitably resist many steps in the treatment process, as well as be a difficult patient in such practical matters as payment, punctuality, and reliability. As noted earlier, a collaborative approach can help solve some of these problems. For example, it is important, after explaining the rationale for using a psychotherapeutic method or assigning homework, to invite the patient to describe how, in his opinion, the method or task will be useful in achieving his goals. It is optimal to get patients to set their own “mini-goals,” but you should not expect them to do so at the very beginning of treatment. To reduce the therapist's frustration, it is helpful to view the behavior of patients with PPD as the result of learning maladaptive behavior patterns, rather than taking their actions personally. Passive-aggressive individuals are difficult to work with, but progress is achievable, and it is always rewarding to see patients begin to behave more appropriately.
Possible complications
The main negative consequence of passive-aggressive disorder is social maladjustment. People around the patient, due to constant negativism, attempts at sabotage and denial of responsibility, begin to move away from communicating with him. This confirms his confidence in his own thoughts and leads to increased symptoms.
Depressive patterns occur in 50-60% of patients. They tend to constantly progress and significantly worsen the prognosis. Alcoholism and drug addiction develop against the background of a negative perception of the world around us. Patients use them to avoid reality. The ability to hide behind an imaginary euphoria allows them to break out of the vicious circle, at least for a while.
Psychosomatic disorders are characterized by the occurrence of symptoms of diseases of internal organs against the background of psychological disorders. Patients with passive-aggressive behavior complain of discomfort, chest pain, frequent headaches, dizziness, and sensory disturbances in the extremities. When examined by a neurologist or performed an instrumental examination, there are no organic disorders, which confirms the psychosomatic nature of the symptoms.
Causes
It is believed that this is a polyetiological disease. Genetic predisposition plays a major role. This theory is supported by clinical studies conducted in the 1970s and 1980s. When studying the anamnesis of patients with a similar mental disorder, it was found that the incidence of symptoms of the disease is 5 times higher in children whose parents suffered from a similar pathology.
Considerable importance is also attached to exogenous organic lesions of the brain during intrauterine development, during childbirth or infancy. These injuries are not severe enough to cause significant symptoms of neurological disease, but are sufficient to impair mental functioning.
Diagnostics
The International Classification of Diseases (ICD-10) classifies passive-aggressive disorder as “other specific personality disorders” (F60.8). To be diagnosed, a person must have at least 5 of the following symptoms:
- constantly postponing work until later;
- gloominess, gloominess and irritability that arise when asked to do something;
- taking on obligations, but not fulfilling them due to “forgetfulness”;
- useful advice from others that can increase work productivity causes dissatisfaction and indignation;
- people in power are criticized, and their success is explained by a trivial coincidence of circumstances;
- disagreement with the assessment of one’s own work, despite its objectively low quality;
- performing tasks slowly or deliberately introducing inaccuracies in them. This refers to work that a person does not want to do.
All patients with personality changes are advised to consult a neurologist. An examination by a specialist makes it possible to exclude organic causes of disorders, for example, tumor pathology, the consequences of cerebral ischemia, and others. To do this, the patient undergoes an EEG (electroencephalography), computed tomography or magnetic resonance imaging.
When making a diagnosis, differential diagnosis is carried out with other personality disorders, primarily with borderline and hysterical. The main difference is the lack of drama and entertainment, as well as the passive nature of aggression towards people.
Diagnosis of the disorder
The disorder is diagnosed based on a conversation with the person and a life history. To assess the degree of disregard for responsibilities and neglect of established rules, social conditions and cultural norms of a particular region are taken into account.
Dissocial personality disorder is diagnosed when the general manifestations of the disorder and specific symptoms are present:
- the disorder is initiated at an early age (up to 15 years), there are no alternating periods of exacerbation and recovery;
- constant conscious violation of social norms, laws, disregard for the rights and feelings of people;
- a person loses his temper easily, is angry, prone to violence;
- there is no feeling of guilt and responsibility for one’s actions;
- tendency to constant lies, fraud and manipulation;
- condemnation of other people's actions, justification and rationalization of one's own;
- lack of planning, impulsiveness of actions, irresponsibility.
The disorder can be differentially diagnosed with the following diseases:
Narcissistic personality disorder
. The person is incapable of empathy, tends to exploit others for his own purposes, but is not aggressive. Patients with narcissistic disorder have difficulty managing their sense of self-worth and value praise and belonging to special groups of people. To maintain their sense of superiority, they devalue other people and their achievements. They overestimate their abilities and exaggerate their achievements. Patients with antisocial personality disorder use others for material gain, while those with narcissistic personality disorder exploit others to maintain their self-esteem.
Borderline personality disorder
. Patients with BPD are prone to manipulative behavior, the purpose of manipulation is to gain attention and support, not material gain. Patients experience intense fear or anger when they feel ignored or rejected, afraid of being abandoned, or being left alone. They often and abruptly change their point of view; there is a phase of idealization and devaluation. They empathize only if they are sure that this person will come to their aid at any moment and will not leave them alone. After the end of the outburst of anger, he experiences a feeling of guilt and shame, convinces himself how bad a person he is.
Behavioral disorders
. Destructive patterns of behavior, in violation of norms and laws, occur up to 15 years of age and cease with adulthood. In about a third of cases they persist, with symptoms consistent with dissocial personality disorder. The disorders are characterized by persistent unsociable, aggressive, defiant behavior patterns. The diagnosis is based on patterns of behavior that include excessive conflict, deceit, cruelty to other people and animals, damage to property, etc. The presence of such pronounced signs is sufficient for diagnosis, but specific actions are assessed only in conjunction with other factors.
Psychopathy
. A disease with pronounced antisocial behavior, with complete preservation of thinking. Sociopathy is a more mildly expressed psychopathy. With a normal existence in society, but complete disregard for the rules and laws, we are talking about sociopathy. Psychopaths also know how to manipulate others, do not form attachments, and need other people only to achieve their goals and have fun. But if a psychopath is inclined to calmly build and implement his plans, then a sociopath acts spontaneously and often commits risky actions.
Substance addiction
. Impulsivity and irresponsibility can result from substance use. The analysis is carried out based on the patient's medical history. Addiction can accompany dissocial disorder or be an independent disease.
Heboid schizophrenia
. The presence of pronounced emotional changes and early-onset emotional dullness is often a sign of slowly developing schizophrenia with heboid manifestations or chronic mania. The leading place in the manifestations of the heboid state in schizophrenia in adolescence is occupied by psychopathological disorders, which contribute to a strong distortion and exaggeration of the typical manifestations of puberty (the desire to assert oneself, a tendency to opposition, contradicting others). Under the influence of the disorder, ordinary manifestations become psychopathological, total negativism and opposition to others and discipline develop.
Dissociative identity disorder
. Type of dissociative (conversion) disorder. Characterized by the presence of two or more alternating personalities (alter personalities, ego states or identities). Dissociative identity disorder is accompanied by involuntary withdrawal from reality, derealization, and depersonalization. Inability to remember events from daily life, certain personal information, traumatic events, or severe stress. The cause of conversion disorder is almost always psychological trauma in childhood or adulthood. As a result of identity disorder, a person finds himself in one or more personalities simultaneously or in turn. At such moments, a person disconnects from himself and stops feeling his own body, and may not see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments and have completely different behavior and habits.
Emotionally unstable personality disorder
. Such people are prone to impulsive actions, are not afraid of consequences, are unpredictable, conflictual and capricious. They have a tendency to have outbursts of emotions and are unable to control their hot-tempered behavior. There are two types of disorder: the impulsive type (emotional instability and lack of emotional control) and the borderline type (characterized by a disorder of self-perception, goals and aspirations, a constant feeling of emptiness, tension and instability of interpersonal relationships, self-destructive behavior, suicidal attempts are possible).
Treatment of passive-aggressive personality disorder in Moscow
Treatment of the disease is difficult, since the patient does not consider his behavior to be the cause of social maladaptation, which reduces adherence to treatment. Many patients perceive visiting doctors as their own humiliation. At the same time, they retain internal hostility towards specialists.
The main method of treating passive-aggressive personality disorder in Moscow at the psychiatric department of Dr. Isaev’s clinic is psychotherapy. Various areas of psychotherapeutic assistance are used here. The work begins with individual sessions, when the psychotherapist helps the patient understand the pathological nature of his thinking and attitude to the surrounding reality.
Regular meetings with a psychologist and psychiatrist are helpful. Working with attitudes allows you to change many of the patient’s values and foundations and return his thinking to a positive direction. After individual sessions, group psychotherapy is indicated to consolidate the results of treatment. It lasts from one year or more.
During sessions with a doctor, the patient becomes aware of the negative consequences of his behavior. Working on the nature of thinking and creating new mechanisms for responding to stress eliminates the pathological symptoms of a personality disorder. The most effective are social skills training and group work through dangerous moments.
Medications are rarely used for passive-aggressive personality disorder. Antidepressants (Fluoxetine and other serotonin reuptake inhibitors) are used for severe depression, which independently worsens the patient’s social and professional adaptation. In addition to them, doctors can prescribe adaptogens that increase the overall tone of the body.
Principles of treatment for impulsive disorder in adults
In most cases, therapy is carried out on an outpatient basis. Treatment begins with the prescription of benzodiazepine drugs and lithium-based drugs. For frequent attacks of rage, doctors at the Leto clinic recommend inpatient therapy using high doses of antipsychotics.
After eliminating internal tension and stabilizing the general psycho-emotional status, the patient is transferred to antidepressants and non-benzodiazepine sedatives. At the same time, a course of psychotherapy is started. A specialist helps a person control emotions, restrain attacks of rage, and respond adequately to the words and actions of other people.
Various muscle relaxation techniques and breathing exercises are effective. For some patients, strength sports, boxing, wrestling are a good way to relax; others are more suited to yoga or Pilates, or morning jogging.
Don't try to cope with impulsive disorder on your own! Call our medical center on a 24-hour anonymous phone number 8(969)060-93-93 and make an appointment for a consultation. Our specialists know very well how to treat the syndrome and have extensive experience working with such patients!
Prevention of the disorder
Prevention of passive-aggressive personality disorders is based on general recommendations that are recommended for all parents and loved ones to follow:
- Provide the patient with a positive emotional atmosphere, acceptance of the child at all stages of growing up.
- Avoid overprotection and authoritarianism in decision making. Infantilism and other characteristic signs of a personality disorder develop due to the child’s inability to independently solve emerging difficulties and make choices in everyday affairs.
- Avoid stressful situations. Children often experience stress: when studying at school, adapting among their peers. Parents should support the child and help him make the right decisions without exerting psychological pressure.
The development of passive-aggressive behavior is facilitated by bad habits - drinking alcohol and taking drugs. Teenagers and adults are advised to completely exclude them from their lives.